As A Life Health Group, we aim to provide the latest information and treatment methods in women’s health. Structural problems within the uterus can negatively affect the quality of life for many women, disrupt reproductive health, and cause menstrual irregularities. One of the most preferred current treatments for these issues is hysteroscopic resection. This minimally invasive surgical technique allows for the safe treatment of intrauterine problems such as fibroids, polyps, adhesions, or septum, offering patients a secure, fast, and comfortable recovery process.
In this guide, you will find comprehensive information about hysteroscopic resection, including what it is, who it is suitable for, its advantages, how it is performed, preoperative and postoperative processes, risks, long-term outcomes, and the treatment approach at A Life Health Group.
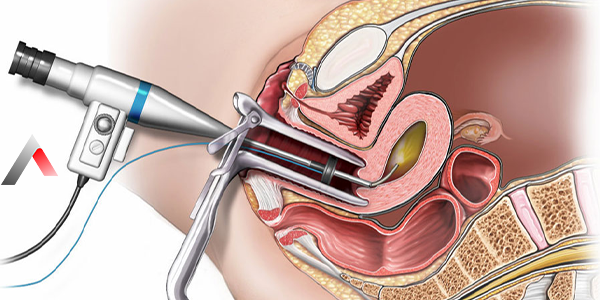
Hysteroscopic resection is a minimally invasive surgical method used for both the diagnosis and treatment of intrauterine problems. A thin, telescope-like device called a hysteroscope is inserted through the cervix, allowing direct visualization of the uterine cavity.
The tip of the hysteroscope contains both a camera and surgical instruments. While viewing the images on a large screen, the doctor can simultaneously remove the problematic tissues inside the uterus. Unlike traditional open surgery, no abdominal incision is made, making the procedure more comfortable, shortening the recovery period, and reducing the risk of complications.
Hysteroscopic resection is especially effective for issues confined to the uterine cavity. This minimally invasive approach is considered one of the most significant advances in modern gynecological surgery and contributes to both the physical and psychological recovery of patients.
Hysteroscopic resection can be applied to resolve a variety of intrauterine problems. The most common indications include:
The most appropriate treatment method varies for each patient. Hysteroscopic resection is particularly preferred for women who have the following conditions:
The procedure is especially effective for women with problems limited to the uterine cavity. For deeply embedded or large fibroids in the uterine wall, laparoscopic or open surgery may be necessary.
The key advantages of hysteroscopic surgery include:
Additionally, the minimal invasive technique allows patients to experience less psychological stress and return to work and social life more quickly.
The procedure is generally carried out in the following steps:
Administration of Anesthesia: General anesthesia is most commonly used, though spinal anesthesia may be applied in certain cases.
Insertion of the Hysteroscope: A thin device containing a camera and surgical instruments is inserted through the cervix into the uterine cavity.
Visualization of the Uterine Cavity: The camera allows detailed examination of the uterine cavity.
Removal of Problematic Tissue: Fibroids, polyps, septum, or adhesions are excised and removed using surgical instruments.
Completion of the Procedure: After resection, the hysteroscope is withdrawn, concluding the procedure.
The average duration of the surgery ranges from 30 to 60 minutes, depending on the size and number of tissues to be removed.
Proper preparation before surgery is crucial for a successful operation. Patients are generally expected to complete the following steps:
Psychological preparation is also important. Providing patients with detailed information about the procedure reduces anxiety and facilitates a smoother recovery process.
The recovery process is generally quite comfortable:
Most patients can return to work and social activities within 1–2 weeks. Regular follow-up visits help minimize complication risks and ensure the uterine cavity remains healthy.
As with any surgical procedure, hysteroscopic resection carries certain risks:
When performed by experienced surgeons, these risks are very low. Additionally, proper preoperative preparation and postoperative care can minimize complications.
Studies show that hysteroscopic surgery achieves high success, particularly in treating polyps and small fibroids. Most women experience improvement in menstrual irregularities, increased fertility chances, and a significant enhancement in quality of life.
Although the recurrence risk is low, regular gynecological follow-up is essential. Long-term monitoring is especially critical for patients with a history of infertility when planning future pregnancies.
At A Life Health Group, we apply the most up-to-date methods in women’s health surgery:
For more information about hysteroscopic resection, please contact us!
At A Life Health Group, we are here to determine the best treatment option for you and guide you through the hysteroscopic resection process. We look forward to seeing you!
Last Updated: 6 Kasım 2025 14:05
Publish Date: 28 Eylül 2024 04:47

Please fill in the fields below so that we can reach you
We are here for all your questions and problems 24/7.